|
In a bustling neighborhood of Riyadh, the parents of a family of five from India had long been an integral part of a local manufacturing firm. For years, their healthcare needs, from managing chronic conditions like diabetes to routine check-ups, were well understood by the AI-assisted system used by their employer's health services. This AI, trained on historical health data reflecting the Indian family's patterns and those similar to them, seemed to provide precise and timely medical interventions. But times changed. As economic tides shifted, the family returned to India and is replaced by another family of five from Pakistan as new expatriates in the Saudi capital city with distinct backgrounds, health profiles, and healthcare behaviors. The AI system, still relying on its original training from the Indian family’s data, struggled. It overlooked new health conditions prevalent in the Pakistani family's community and failed to recognize new patterns of healthcare needs tied to their different employment sector and cultural practices and lifestyle. This story is emblematic of a key challenge in the use of AI in Saudi Arabia's healthcare sector despite the impressive strides the kingdom has taken in recent after the launch of Vision 2030 in 2016. This challenge is about the transient and evolving nature of the expatriate population. The substantial and growing expatriate population in Saudi Arabia—rising from 14.5 million in 2023 to about 15.7 million in 2024 and representing 75.6% of total population growth—adds critical complexity to the issue of AI generalizability in healthcare AI systems. 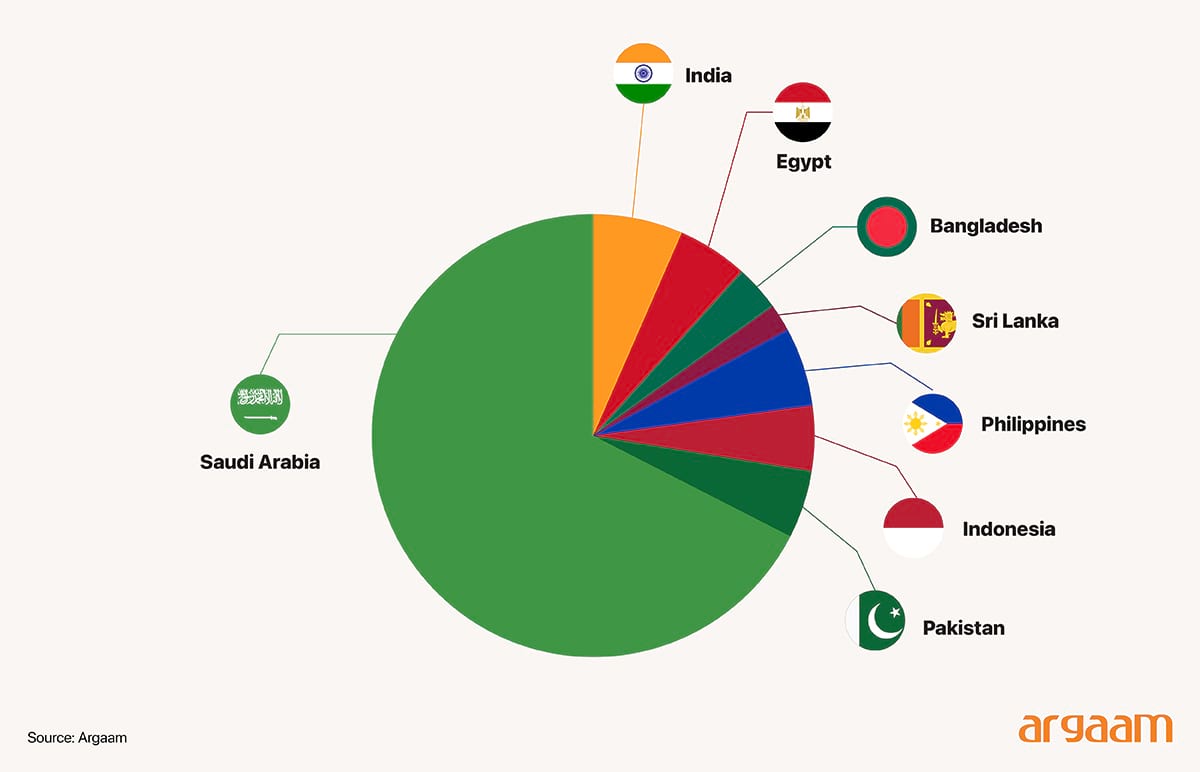
Expat populations often come from varied ethnicities and genetic backgrounds that may differ considerably from native Saudis. AI models trained predominantly on data from Saudis or other homogeneous populations may fail to generalize accurately across this diverse group with potentially different disease prevalence, clinical presentations, or genetic predispositions. This mismatch risks diagnostic inaccuracies. To ensure generalizability, AI systems require training and updating datasets that represent the true clinical and demographic diversity of the population, which helps enhance the use effective use of AI in various pioneering initiatives across key hospitals.
Saudi Arabia’s pioneering efforts in the region to integrate artificial intelligence into healthcare represent a forward-thinking approach to enhancing medical diagnostics and patient care. 
The King Abdullah University of Science and Technology and the Saudi Data and Artificial Intelligence Authority (SDAIA) have jointly launched MiniGPT-Med, an advanced vision-integrated AI language model capable of identifying 14 different diseases. The King Faisal Specialist Hospital & Research Center leveraged AI to generate CAR-T cells for cancer treatment and conducted 7,000 whole genome sequencing tests to assess genetic predispositions. SDAIA partnered with King Khaled Eye Specialist Hospital to develop "Eyenai," an AI solution to detect diabetic retinopathy. 
The Seha Virtual Hospital in Saudi Arabia has tied up with South Korean healthtech firm Lunit to provide AI-powered solutions for breast cancer and tuberculosis screening. King Abdulaziz City for Science and Technology (KACST) has developed an AI system to segment brain tumors for improved accuracy on MRI scans. 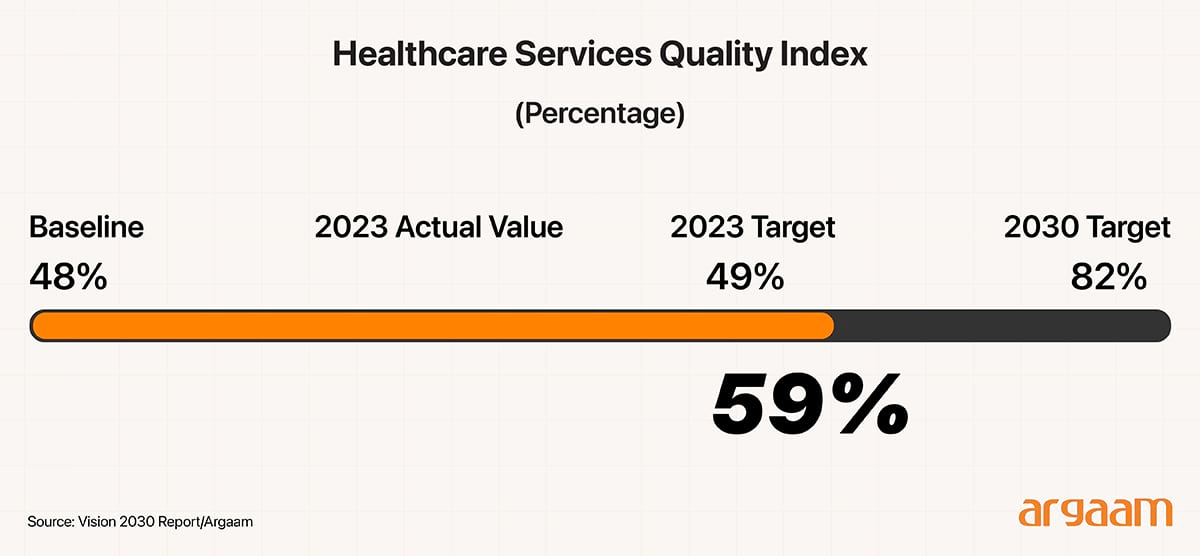 
Evolving Data, Evolving Costs
Implementing an AI diagnostic tool in a dynamic healthcare setting involves more than just the initial investment. In particular, maintaining its accuracy and effectiveness requires regular updating of the underlying data to reflect evolving patient characteristics. This ongoing data collection, cleaning, and integration process entails significant costs that must be carefully considered to ensure the AI tool continues to provide reliable clinical decision support over time. Let’s have this hypothetical example to explain the hidden costs behind keeping AI up to date. A large healthcare system in that decides to implement an AI diagnostic tool to improve clinical decision-making. The initial investment for developing, deploying, and training staff to use the AI amounts to $2 million. While this upfront cost covers the AI's launch, the story doesn’t end there. Because the expatriate population served by the system is dynamic and continually evolving, the characteristics of the community—their health profiles, prevalence of diseases, and care-seeking behaviors—are in constant flux. To ensure that the AI remains accurate and effective for this changing population in the kingdom, the healthcare system must retrain and update the model annually. Each year, this process entails significant expenses. First, the collection and cleaning of fresh data that captures the latest health trends within the expatriate community costs around $200,000 (just for explanatory purposes in this analysis). Then, the AI model itself must undergo training and validation to adapt to new information, which requires another $300,000. On top of this, the system must fund staff training and provide ongoing IT support to help clinicians effectively use the updated AI tool, adding a further $100,000. Altogether, these annual updates total $600,000. Over a five-year period, these recurring costs accumulate to $3 million, on top of the original $2 million investment. Therefore, by the end of five years,the healthcare system will have spent approximately $5 million to not only implement but also maintain the AI diagnostic tool tailored for its evolving expatriate population. This example underlines a crucial point: maintaining the relevance and accuracy of AI in a fast-changing and diverse population requires substantial financial commitment beyond the initial purchase.
One image, two realities
Another example which’s often used in academic research about the issue of AI generalizability in healthcare is the ‘single image’. A single image taken in two different clinical settings can shape the success or failure of AI tools in diagnosing a diabetic patient. When captured in a well-equipped urban hospital with optimal lighting and high-resolution cameras, the image provides clear and accurate data for the AI to analyze, leading to reliable identification of diabetic retinopathy or other complications. If the image is taken in a rural or less-resourced clinic in a remote area, where lighting conditions are poorer, the equipment is less advanced, the AI may struggle to interpret the data accurately. This can lead to missed diagnoses or false negatives, undermining the AI’s effectiveness. This situation highlights a fundamental challenge with AI generalizability: for algorithms to perform reliably across settings, training data must be representative of the heterogeneity found in target environments, including geographic, demographic, and technical diversity. Without this, AI tools risk failing to accurately diagnose conditions like diabetic retinopathy, potentially missing cases or generating false positives. In conclusion, health systems must carefully consider these ongoing costs when planning and assessing the value of AI technologies, ensuring that budgets and health technology assessments reflect the full scope of investment needed to achieve meaningful, sustained benefits. The generalizability and real-world applicability of AI tools in medicine remain complex and context-dependent challenges. Evidence often relies on retrospective or narrowly defined datasets that may not reflect the diversity and variability of clinical settings. |
|
|
|
|
|






